By C. Alan Hopewell, PhD, MP, ABPP, BSM, MAJ (RET) Robert Klein, PhD, CPT US Army and Michael Adams, PhD, LTC (RET)
*This is an article from the Winter 2024 issue of Combat Stress
Fort Hood is a United States Army Post located in Killeen, Texas. This post was originally named for Confederate General John Bell Hood, but has since been renamed Fort Cavazos after General Richard E. Cavazos, a native Texan and four-star general. However, since all of the research reported here was conducted at Fort Hood during the Global War on Terror (GWOT,) the name Fort Hood will be referenced. The main cantonment of Fort Hood had a total population of 53,416 as of the 2010 U.S. census and at the time of this original research, was the most populous U.S. military installation in the world.1 In April 2014, the Post’s website listed 45,414 assigned soldiers and 8,900 civilian employees covering an area of 214,000 acres (87,000 hectares).
In 2001, the War on Terror became a prime focus of post activities. Fort Hood transitioned from an open to a closed post with the help of military police from Army Reserve units. The post is also the headquarters of III Armored Corps and First Army Division West and is home to the 1st Cavalry Division and 3rd Cavalry Regiment, among others. During GWOT and the time period of research conducted, the 4th Infantry Division was also stationed at Fort Hood, making it the largest military deployment platform in the world.1 As a consequence, the outpatient psychiatry/ behavioral health operations were the largest in the world at the time. During the height of the Iraqi Surge, more than 400 Soldiers were seen or were attempted to be seen per day at the Carl R. Darnall (CRDAMC) Resilience and Restoration Center (the post outpatient clinic for psychiatry and behavioral health), more patients than were seen at the CRDAMC Emergency Department per day. During the research period reported in the article, CRDAMC was upgraded in its designation to an Army Medical Center and a special Washington D.C. commission coordinated by the senior author resulted in essentially tripling the staffing of the CRDAMC Resilience and Restoration Center.

The Resilience and Restoration Center as consolidated by COL Lorree K Sutton, Carl R. Darnall Hospital Commander.
A number of Fort Hood units were deployed to Afghanistan in support of Operation Enduring Freedom and to Iraq for Operation Iraqi Freedom during the GWOT. In December 2003, the 4th Infantry Division captured Saddam Hussein. In the spring of 2004, the 1st Cavalry Division followed the 4th Infantry Division deploying to Iraq. These divisions then generally rotated through the deployment cycle, with the Restoration and Resilience Center supporting deploying troops and aiding the returning troops with their mental health needs and re-adjustment to garrison in rotation. In 2009, Fort Carson, Colorado‘s First Army Division West re-stationed to Fort Hood in order to consolidate its mission to conduct Reserve Component mobilization training and validation for deployment, switching places with 4th Infantry Division, which then relocated to Fort Carson.
It was into this situation that the senior author reported to CRDAMC in June of 2006 and assumed the position of Officer-in Charge (OIC) of the Restoration and Resilience Center. The second author served as a Psychology Intern and the third author as Chief of Behavioral Health during this time period respectively. Half of the CRDAMC psychiatrists and psychologists were deployed during this interval, primarily with the 4th Infantry (Ivy) Division, leaving only one active-duty psychiatrist and one civilian psychiatric employee to serve all of CRDAMC, in addition to only four psychologists to cover a health care cohort of easily over 50,000.
The senior author had volunteered to return to active duty, as he was one of the only senior clinical psychologists in the United States who was both a Clinical Neuropsychologist and who also had substantial prior military experience. He was also the only Army Medical Neuropsychologist with a pharmacology degree who could manage patient medications, for which he was awarded the Bronze Star Medal after his service in Iraq. He was specifically returned to active duty as he had previously established the Traumatic Brain Injury Clinic (TBI) at Landstuhl Army Regional Hospital and was the de facto Army expert on brain injury and concussions.2 He had also been the Chief of Neuropsychological Services at Brooke Army Medical Center from 1981 through 1983 before being assigned to the Individual Ready Reserve (IRR). For these reasons, he was chosen on his return to active duty by the Vice Chief of the Joint Chiefs of Staff and the Psychology Consultant to the Army to be assigned to CRDAMC and ultimately to deploy in support of Operation Iraqi Freedom.
Upon assuming duties at CRDAMC, the Hospital Commander, COL Loree K. Sutton, requested that the senior author design and implement surveys designed to determine the mental health care needs of the garrison Soldiers and to document the need for increased mental health services. This was particularly needed in terms of the marked increase in diagnoses of post-traumatic stress disorder (PTSD) and traumatic brain injuries (TBI). As part of that request, returning Soldiers needing services were referred to the Restoration and Resilience Center for mental health treatment, most of them from the returning 4th Infantry Division. These Soldiers were thereafter systematically screened, not only for general mental health needs, but also specifically for traumatic brain injuries which were then occurring with increasing frequency in the wartime theaters as a result of improvised explosive device (IED) blast injuries.

LTC Michael Adams, COL Wilma Larsen, and COL Lorree K. Sutton presenting the senior author with an award in recognition for TBI and PTSD screening procedures.
As part of the education of CRDAMC and Restoration and Resilience Center staff at the time in regard to blast injuries / concussion or mild traumatic brain injuries / (mTBI), some of the following guidance from the Centers for Disease Control (CDC)3 were followed:
Blast Injuries: Essential Facts / Key Concepts:
- Bombs and explosions can cause unique patterns of injury seldom seen outside combat.
- Expect half of all initial casualties to seek medical care over a one-hour period.
- Most severely injured arrive after the less injured, who bypass EMS triage and go directly to the closest hospitals.
- Predominant injuries involve multiple penetrating injuries and blunt trauma.
- Explosions in confined spaces (buildings, large vehicles, mines) and/or structural collapse are associated with greater morbidity and mortality.
- Primary blast injuries in survivors are predominantly seen in confined space explosions.
- Repeatedly examine and assess patients exposed to a blast.
- All bomb events have the potential for chemical and/or radiological contamination.
- Triage and lifesaving procedures should never be delayed because of the possibility of radioactive contamination of the victim; the risk of exposure to caregivers is small.
- Universal precautions effectively protect against radiological secondary contamination of first responders and first receivers.
- For those with injuries resulting in nonintact skin or mucous membrane exposure, hepatitis B immunization should be administered (within 7 days) and age-appropriate tetanus toxoid vaccine (if not current).
Blast Injuries
- Primary: Injury from over-pressurization force (blast wave) impacting the body surface — Tympanic membrane rupture, pulmonary damage and air embolization, hollow viscous injury. (a sudden and pronounced rise in intra-abdominal pressure can rupture a hollow viscus).
- Secondary: Injury from projectiles (bomb fragments, flying debris) — Penetrating trauma, fragmentation injuries, blunt trauma.
- Tertiary: Injuries from displacement of victim by the blast wind — Blunt/penetrating trauma, fractures, and traumatic amputations.
- Quaternary: All other injuries from the blast — Crush injuries, burns, asphyxia, toxic exposures, exacerbations of chronic illness.
Primary Blast Injury
Lung Injury
- Signs usually present at time of initial evaluation but may be delayed up to 48 hours.
- Reported to be more common in patients with skull fractures, >10% BSA burns, and penetrating injury to the head or torso.
- Varies from scattered petechiae to confluent hemorrhages.
- Suspect in anyone with dyspnea, cough, hemoptysis, or chest pain following blast.
- CXR: “butterfly” pattern.
- High flow O2 sufficient to prevent hypoxemia via NRB mask, CPAP, or ET tube.3

Typical IED Blast in Iraq 2008. One of the Senior Author’s Patients Treated by the 785th Combat Stress Company, Camp Liberty, Iraq.
The Global War on Terrorism (GWOT) brought to the forefront the issue of the relation between mild traumatic brain injury (mTBI) and combat-induced post-traumatic stress disorder (PTSD). The two are related because of the similarities in how soldiers incur mTBI and/or PTSD. Soldiers are frequently exposed to concussive blasts related to improvised explosive devices. In and of itself, being exposed to an IED blast meets the Diagnostic and Statistical Manual of Mental Disorders-Fourth and Fifth Edition-Text Revised (DSM-IV- V – TR) Criterion A1 for PTSD and can potentially cause mTBI due to concussive blast. It should be noted that the DSM-IV-TR was the version of the DSM at the time of the major part of GWOT and this research. Additionally, the empirically-based published literature at the time of the screening will only be used to give the reader an understand of the state of scientific thought during the GWOT.
As a resident from 1975 – 1976, the senior author had also been the very first student and Senior Resident of Harvey Levin, PhD, who co-directed the formal traumatic brain injury (TBI) program in the Division of Neurosurgery at the University of Texas Medical Branch, Galveston (UTMB). Based upon this early work with TBI models, Levin et al. suggested that post-concussional symptoms occur along three dimensions; somatic, cognitive, and affective. Somatic symptoms include headache, dizziness, vision difficulty, and deficits in balance and motor functioning, as well as a number of additional symptoms.4 Neurocognitive sequelae consist of deficits in attention/concentration, memory, cognitive processing speed, fatigue, and impairment in both simple as well as complex reaction time.5, 6 Typical affective symptoms can include anxiety, depression, irritability and mood swings. The documentation of such symptoms by Harvey Levin and Hopewell at the UTMB – the official Traumatic Brain Injury program at the time for the State of Texas,7 led to the eventual development of the Neurobehavioral Symptom Inventory as a brief screening effort to record most of the typical symptoms associated with concussions.8
Most civilian TBI injuries are acceleration / deceleration impact inertial related such as occur in motor vehicle accidents. However, blast injuries appear to be better described as a fluid percussion model. In this regard, a fluid percussion model of brain injury is similar to an IED related concussive blast and has also been studied in animals and used to hypothesize changes in people with mTBI. “Human blast injury studies in organs other than the brain have shown that at least two atmosphere percussion waves in the fluid media of the brain can produce mTBI findings similar to findings in animal studies.”9 Over-pressure waves have been associated with producing diffuse axonal injury (DAI) via rapid acceleration and deceleration (coup-countercoup). DAI is associated with the shearing or damaging of axons that project from the brain stem. If the coup-countercoup action is severe enough it can cause a loss of consciousness (LOC). When LOC is experienced, a Soldier can further harm the brain by making significant contact with a physical object such as a weapon, vehicle structure, or the ground as he or she falls.
PTSD is amongst the most controversial diagnoses included in the DSM-IV-TR.10, 11, 12 The controversy with PTSD revolves around the boundaries of the disorder, diagnostic criteria, central assumptions, clinical utility, and prevalence in various populations.10- 12 Spitzer et al., Gold et al., and Boals and Schuettler arrived at conflicting results when looking at the importance of Criteria A1 and A2 in defining PTSD. Gold et al. reported that higher levels of PTSD symptoms were associated with non-traumatic events than traumatic events when scoring results were based on classification by coders.11 On the other hand, Boals and Schuettler found that PTSD symptoms were more associated with traumatic events than non-traumatic events when scoring results were based on participants’ ratings.12 Further Boals and Schuettler reported that Criterion A1 had a minimal relation to PTSD symptoms when A2 was considered.12 These two conflicting studies bring in to question the validity of Criteria A1 and A2 in diagnosing PTSD.
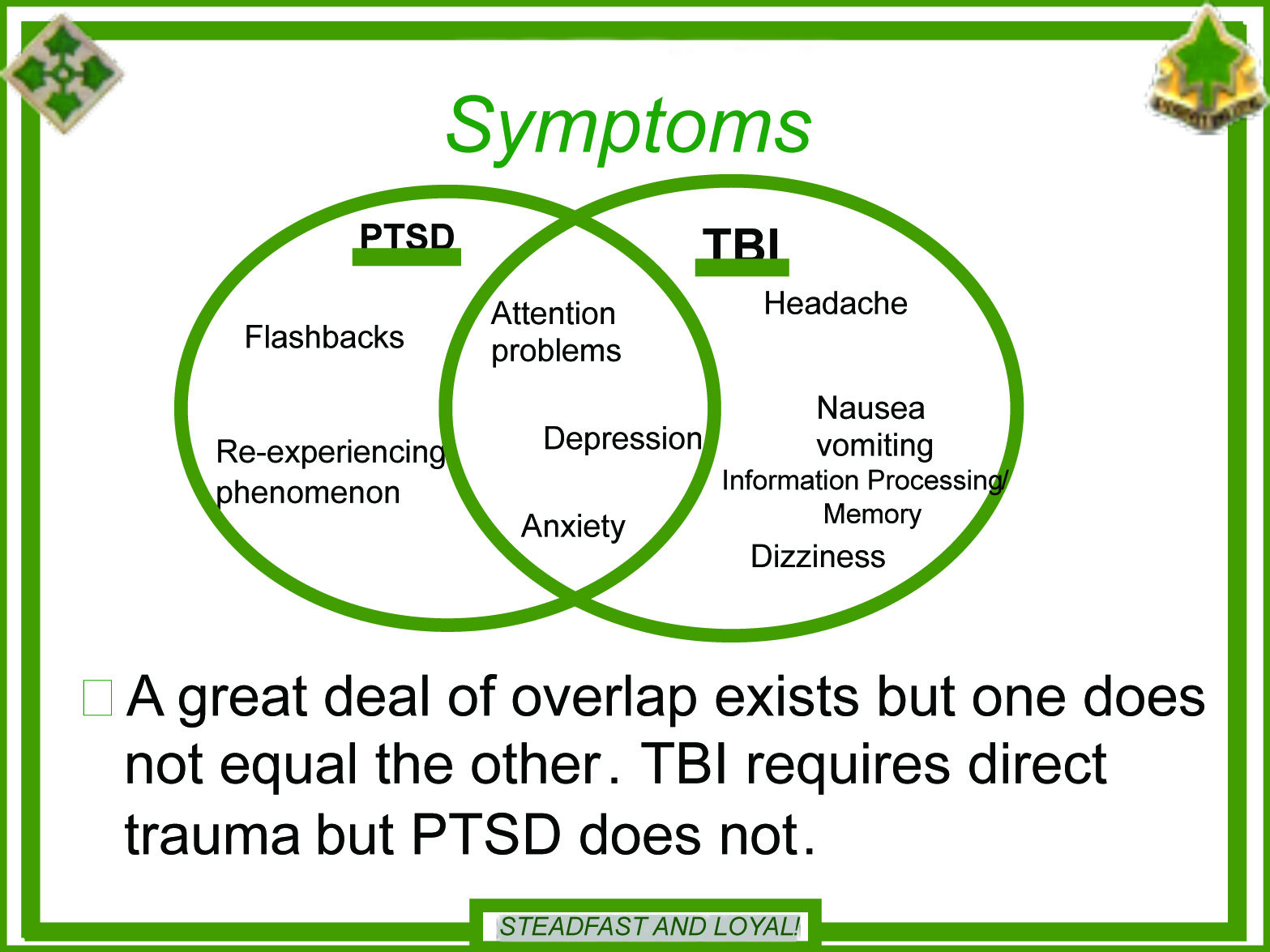
Overlapping symptoms between mTBI and PTSD can complicate the differential diagnosis process and lead clinicians to wonder whether they should ascribe a person’s clinical presentation to a diagnosis versus dually-diagnosing. The lack of agreement in the research community regarding which specific PTSD and mTBI symptoms overlap further complicates diagnosis.13,14 Defense Veterans’ Brain Injury Center (DVBIC) considers depression, anxiety, and attention difficulties as overlapping symptoms. Depression, anxiety, and sleep are non-neuropsychological overlapping symptoms of post-concussional syndrome (PCS) and PTSD that the ICD-10 and DSM-IV-TR agree upon. The Veterans Administration considers concentration difficulty, sleep difficulty, irritability, and social withdrawal as overlapping symptoms. Further complicating the differential diagnosis process is the overlapping symptoms between anxiety and major depression, which are common behavioral symptoms of mTBI and PTSD. These overlapping symptoms consist of problems with sleep, concentration, and fatigue as well as psychomotor/arousal symptoms.15 Other research suggests that irritability, attentional dysfunction, difficulty concentrating, amnesia, decreased cognitive processing, and sleep disturbances are overlapping.9,16
There are issues with accurately measuring both PTSD and mTBI primarily because symptoms are subjective, can be exaggerated, and can demonstrate considerable overlap. When a client endorses a symptom on a self-report measure it is up to the clinician to determine the etiology of the symptom. For example, if a person endorses experiencing headache, the clinician needs to determine whether the headache is tension-based (i.e., psychiatric-etiology) or is a posttraumatic headache. Just because a person has a headache does not mean it is a headache that is characteristic of a TBI and therefore, can lead to a misdiagnosis of post-concussive syndrome (PCS). In terms of PTSD symptomatology, there is little consensus regarding the best diagnostic cut scores for self-report measure and no research has been conducted to determine optimum cut scores for active-duty service members. A cut score should shed light on to the diagnostic efficiency (i.e., sensitivity and specificity, negative predictive power, and positive predictive power) of an instrument and therefore, aid the clinician in rendering a diagnosis.
Reported symptoms can also be exaggerated due to secondary gain or somatization. It is not uncommon for a soldier to report on an inventory that a symptom is severe, but further investigation reveals that it does not impact their activities of daily living. Most researchers do not conduct item analyses to determine which symptoms discriminate best between those who do and do not have a clinical diagnosis.17, 18 This is important in research when there are diagnoses that share multiple symptoms like PTSD and PCS.
At the self-report psychological instrument level, overlapping symptom between the PTSD Checklist (PCL)19 and Neurobehavioral Symptom Inventory (NSI)20, 21 includes difficulty concentrating, sleep difficulty, irritability, and forgetfulness/trouble remembering. Across cultures, all 16 items on the Rivermead (European version of the NSI) are on the NSI. Loss of balance, poor coordination, hearing difficulty, numbness/tingling, change in taste/smell, change in appetite are items that are not on the Rivermead. There is no universal agreement in the behavioral health community on the specific etiology of post-concussion symptoms in individuals with mTBI. Persistent post-concussion symptoms could be neurological, psychological, or both. The neurological side of the debate documents that post-concussion symptoms are attributed to neurological damage often associated with axonal stretching or injury. The persistence of symptoms is assumed to be due to metabolic and physiologic changes in the brain that have not returned to homeostasis.22 The psychological camp suggests that symptoms are attributed to transient physiological disturbance and are maintained by psychological distress.23, 24 Bazarian et al. showed that post-concussive symptoms are reported more by mTBI patients without positive neurological or radiological findings than patients with moderate or severe TBI.25 Research suggests that a significant risk factor for the development of PCS is three or more prior concussions, which a service member can receive via multiple combat tours.22, 26 This also means that the person has likely been exposed to more psychological trauma with increasing numbers of both combat tours and blast exposures.
Some of the variance in the literature related to post-traumatic stress and neurobehavioral symptoms is also likely due to a combination of conceptualization problems and measurement issues. As previously mentioned, there are no universally accepted diagnostic criteria for assigning a diagnosis associated with mTBI and there is no “gold standard” for post-concussive symptoms. With regards to PTSD, there is some question about whether a person needs to be conscious to develop PTSD and there is no universally accepted structure of PTSD. Some of the variance involved in the different structures may also be due to researchers using different instruments to measure PTSD (i.e. PCL and CAPS).
The VA/DoD Clinical Practice Guideline for the Management of Post-Traumatic Stress states that:
“Post-traumatic stress disorder (PTSD) is the most prevalent mental disorder arising from combat. It also strikes military men and women deployed in peacekeeping or humanitarian missions, responding to acts of terrorism, caught up in training accidents, or victimized by sexual trauma. Its burden may be transient or last a lifetime. The response to psychological trauma is probably as old as human nature but the diagnosis of a traumatic stress disorder is among the newest in the diagnostic catalogue. Twenty years ago, most people, including most clinicians, did not know that PTSD existed. Even among those who acknowledged PTSD, their view tended to be retrospective: PTSD planning and practice in the Departments of Defense (DoD) and Veterans Affairs (VA) centered on work with survivors of past conflicts such as Vietnam, Korea, or World War II. As DoD and VA face the challenge of a new generation of combatants and veterans, our perspective must become prospective: building on the lessons of the past and serving those in present need but also aiming at the future in order to maximize preparedness and, if possible, prevention” (2004, pg. i).27
A thorough review of the etiology, nature, effects upon the nervous system, the comorbidity of TBI, and the treatment of PTSD especially after combat is additionally provided in Moore, Hopewell, and Grossman’s book Violence and the Warrior, Living and Surviving in Harm’s Way: A Psychological Treatment Handbook for Pre- and Post-Deployment.28
A screening instrument checking for these symptoms along with the Center for Epidemiological Studies-Depression (CES-D) depression checklist29 and the Traumatic Event Sequelae Inventory (TESI)30 was used to screen Soldiers, mostly from the 4th Infantry Division, for concussion and PTSD, although a few Soldiers who were Veterans of Operation Enduring Freedom in Afghanistan were also screened. The CES-D, originally published by Radloff, is a 20-item measure that pulls for ratings as to how often over the past week symptoms associated with depression have been experienced such as restless sleep, poor appetite, and feeling lonely.29 Response options range from 0 to 3 for each item (0 = Rarely or None of the Time, 1 = Some or Little of the Time, 2 = Moderately or Much of the time, 3 = Most or Almost All the Time). Scores range from 0 to 60, with high scores indicating greater depressive symptoms.
The CES-D also provides cutoff scores (e.g., 16 or greater) that aid in identifying individuals at risk for clinical depression, with good sensitivity and specificity and high internal consistency.31 The CES-D has been used successfully across wide age ranges, is sensitive to differences between caregivers and non-caregivers, and is sensitive to changes in caregiver depressive symptoms after intervention.31, 32 Although the CES-D has somewhat different factor structures across racial and ethnic groups, it can be used appropriately with diverse caregivers.33
The Traumatic Event Sequelae Inventory (TESI) is a special psychometric instrument design to diagnose and quantify a very specific emotional and behavioral symptom spectrum most frequently reported by individuals who has been exposed to traumatic events.30 TESI was developed in 1995 as a focal component of a comprehensive multidimensional psychometric battery for assessment and quantification of emotional injury and psychiatric disability. Originally intended for the commercial market (personal injury/workers’ compensation) the first announcement of TESI appeared in the California CLAIMS Journal, Winter 1996.34 TESI has since become one of the most widely used instruments in the USA for the assessment of posttraumatic emotional and behavioral sequelae, with the military cohort screened resulting in a normative population of over 86,000 subjects. The original TESI items were selected from the actual medical records of patients diagnosed with and treated for trauma-based anxiety disorders from 37 psychiatric inpatient, residential, and outpatient health care facilities in New York, New Jersey, Pennsylvania, California, and Florida. TESI utilizes a dual scoring system, yielding diagnostic accuracy greater than 95 percent. The first system utilizes standardized t-scores developed during the initial standardization of TESI in 1996.30
The second scoring system, with Gradient Frequency Scores (GFS,) or TESI Score Levels, was empirically developed during the second standardization of TESI in 2002, based on the clinical population of 36,340 individuals who have experienced single or multiple traumas and were in treatment for related posttraumatic disorders in a variety of clinical settings. Comprehensive assessments, clinical diagnostic summaries, and psychometric data from follow up assessments were utilized in the development of the Gradient Frequency Scores. Each GFS represents a particular level of TESI raw scores at which significantly different diagnostic classifications are present at the confidence interval of .95, rendering specific interpretive clinical considerations and therapeutic interventions.
The first four GFS levels (1–4) are likely to be indicative of subsyndromal disturbances which may or may not be related to a traumatic event(s). Based on the data available from our normative samples, it was our conclusion that the diagnostic certainty at these levels is not sufficient enough to satisfy the DSM-V or ICD-10 diagnostic criteria for a posttraumatic stress disorder.
The fifth GFS level (5) may indicate a subthreshold form of PTSD, but with insufficient degree of diagnostic certainty to diagnose a full, syndromal level of the disorder. The “rule out” diagnoses at this level should be supported with the GFS scores from other TESI components used in evaluation. Diagnosis of subthreshold post-traumatic disturbances and dysfunctionality is also only possible by using combined battery scores.
The sixth GFS level ( 6) represents the average number of symptoms found among our normative sample, with a range of 1 SD of mean for clinical group and more than 3 standard deviations above mean for non-clinical group. Diagnostic formulation of posttraumatic disorders at this level must be supplemented with the results (GFS scores) from other TESI components.
The seventh and the eighth GFS levels (7 – 8) of TESI’s raw scores represent ranges of symptomatology, characteristic of our normative sample which is sufficiently wide in spectrum to suspect that scores at these levels may involve a more complex clinical picture rather than PTSD as a single, or a focal disorder, or at least a severe level of PTSD. At these levels, either significant psychopathology with etiology other than the trauma may be present. These may be concussions complicated by other medical factors. This may occur when a single concussive episode produces cognitive and affective symptoms which persist and which are influenced or exacerbated by concomitant medical factors such as serious other medical complications, such as chronic pain associated with severe orthopedic injuries, as often happens in a combat Veteran population. These complications are often also further complicated by exacerbating emotional disorders which act as moderating variables. At this level, many concussion survivors demonstrate multifactorial difficulties. In some cases, the presence of self-deception, intentional symptom exaggeration, factitious disorders, malingering, or conscious engagement in cost benefit analysis of injury and its sequelae may be present and must be distinguished from actual injury levels.
Primary Disturbances (PD):
Initial post-traumatic disturbances reported in primary care: Somatic Disturbances, Affective Disturbances, Cognitive Disturbances, Behavioral Disturbances, Marital Disturbances, Occupational Disturbances, Disturbances of General Functionality, Psychomotor Acceleration, Psychomotor retardation, Fear, Dissociative Experiences and Hypervigilance.
Systemic Disturbances (SD):
Systemic Disturbances are disorders diagnosed by various clinical and laboratory methods such as: Cardiological Disturbances, Musculoskeletal Disturbances, Hematological Disturbances, Metabolic Disturbances, Endocrine Disturbances, Gastrointestinal Disturbances, Neurological Disturbances.
Clinical Impairments (CI):
Clinical impairments include subsyndromal, subthreshold, or syndromal short, intermediate, and long-term posttraumatic manifestations of physiological, cognitive, psychological, and environmental disturbances present during the entire duration of trauma integration, synthesis, and diffusion. Some domains of impairments may persist in form of residuals of the integration process, subsequent constitutional vulnerabilities to re-traumatization, or factors rising various disturbances to levels of permanent and stationary disabilities.
TESI Varimax Factors (F):
Individual TESI items (1-39) were factor analyzed to determine which items clustered together in a discernible structure. Given that, by definition, the structure of typical PTSD symptoms is not meaningful for those who do not have the disorder, but only the clinical sample was used in this analysis. Principal components analysis using varimax rotation yielded eight factors with eigenvalues of 1.0 or higher. Factor 1 (eigenvalue=9.19) accounted for 23 percent of the variance. Factor 2 (eigenvalue = 1.99) explained 5 percent of the variance. The remaining factors yielded figures as follows: Factor 3 (eigenvalue =1.44) 3.7 percent; Factor 4 (eigenvalue 1.27) 3.3 percent; Factor 5 (eigenvalue = 1.2) 3 percent; Factor 6 (eigenvalue = 1.1) 2.9 percent; Factor 7 (eigenvalue= 1.1) 2.7 percent; and Factor 8 (eigenvalue 1.0) 2.6 percent. The entire analysis thus accounted for 46.8 percent of the variance. Underlying concepts for these factors might be described as follows:
Factor 1 might best be described as detachment & loss of control;
Factor 2 relates to impaired cognitive abilities;
Factor 3 can be termed physical complaints, primarily related to digestive processes;
Factor 4 captures physical complaints primarily related to anxiety & stress;
Factor 5 taps into ruminations and related dysfunction;
Factor 6 taps into anger and frustration;
Factor 7 relates to psychomotor agitation;
Factor 8 can be labeled “marital problems.”
Overall, the factor structure supports TESI as an instrument which incorporates dimensions relevant to the diagnosis of PTSD. Given the differences in TESI item responses between gender and ethnic groups within the clinical sample, principal component analysis was also repeated separately for each ethnic and gender group. Results indicate that that TESI’s factor structure differs somewhat among these sub-samples. For each group, 9 factors with eigenvalues above 1.0 were derived. Principal component analysis with African Americans accounted for 50.34 percent of the variance. For Latinos, the analysis, accounting for 50.06 percent of the variance. When the analysis included only non-Latino Whites, it accounted for 53.75 percent of the variance. For women, the analysis accounting for 56 percent of the variance. Finally, principal component analysis including only men accounted for 57.6 percent of the variance.
One thousand two hundred and fifteen (1,215) combat Veteran Soldiers were screened with TESI and the CES-D at Carl R. Darnall Army Medical Center, Ft. Hood, Texas, upon their return from a combat deployment to Iraq in support of Operation Iraqi Freedom.35 Most returning Soldiers were from a returning combat infantry unit that was engaged in some of the heaviest fighting in Iraq prior to the successful Surge, although a few were returning Operation Enduring Freedom Veterans. The screenings were done after initial Post-Deployment Health screenings mandated referral to the Resilience and Restoration Center at Darnall Army Medical Center, the outpatient clinic of the Department of Psychiatry and Behavioral Health. The screenings were accomplished in 2007, a time when the Department of Psychiatry and Behavioral Health at Darnall Army Medical Center operated essentially the largest outpatient psychiatry clinic in the world.
The screenings included 966 males and 249 females ranging in age from 18 to 59 years of age.35 104 of the Soldiers were documented to have blast related concussions in addition to a range of psychiatric co-morbid disorders, to include post-traumatic stress disorder (PTSD). Ninety-seven (97) concussed Soldiers were male and seven were female. Verimax factor analyses documented psychiatric factors demonstrated by the Soldiers, with an analysis of combined PTSD and concussion symptoms, comparing Soldiers with and without concussion. Degrees of primary disturbances generally ranged from a low of 33 percent to a high of 68 percent for the sample. The severity of PTSD and concussion injuries, clinical considerations, and varimax factors are discussed. Some of the major findings in terms of demographic composition, TESI scores, and GFS levels are presented below.
Population groups included Anglo/Caucasian, African Americans, Latinos, and Asians, both male and female. Ages ranged from 19 to 59 years of age with mean ages from 24 to 28 years of age, partly as older Reservists had returned to active duty for GWOT. The modal educational level was 12 years. Mean GFS levels ranged from 5.7 for non-injured, non-concussed Soldiers to 6.4 for combat Veterans with injuries and concussions. Caucasians accounted for 64.42 percent of those screened, African Americans for 13.46 percent, Latinos for 11.54 percent, Asians for 1.92 percent, and “Others” for 6.73 percent. Only three of the concussed group had no combat exposure, presumably being injured during non-combat duties. Individuals with concussion scored an average GFS level of 6.4, while Soldiers without concussion scored an average GFS level of only 5.8. The presence of concussion therefore raised the GFS by one level, obviously complicating the underlying PTSD symptoms. This means that in addition to probable PTSD, concussion will substantially increase the comorbidity of damage to the individual injured Soldier. Females also scored higher at a GFS of 6.1, while males scored at the lower GFS level of 5.8, this being consistent with literature indicating that females often experience PTSD at higher or more severe levels than do males.
While primary disturbances ranged from affective to somatic disturbances, those which appeared to affect both the injured as well as the concussed cohorts were those of psychomotor retardation, with fear and affective disturbances interestingly being less problematic. Systemic disturbances for the injured as well as the concussed cohorts were those of musculoskeletal and endocrinological and neurological, respectively, with this being consistent with the conceptualization and likely sequelae of these injuries. Degrees of impairment for the injured as well as the concussed cohorts included communication problems for the former and concentration deficits for the latter, again being consistent with the conceptualization and likely sequelae of these injuries.
As previously noted, the fifth GFS level indicates significant psychiatric disturbance, and may indicate a subthreshold form of PTSD, but with insufficient degree of diagnostic certainty to diagnose a full, syndromal level of the disorder. The “rule out” diagnoses at this level should be supported with the GFS scores from other TESI components used in evaluation and from possibly other evaluations. In an extremely busy military practice with over 400 patient consults a day, Soldiers scoring at this GFS level on TESI could be “triaged” for further PTSD examination. Therefore, the cut off level of the fifth GFS level proved to be very important, as Soldiers scoring less than this could be put more on a regular treatment schedule, while Soldiers scoring 5 or more could be expedited for further and more thorough evaluation.
Soldiers with concussion scoring at the sixth GFS level, could also be expedited for assessment, with additional focus on the TBI aspects of their injury, aspects which, for example, could involve substantially different medication treatment such as for headache, the single most frequent symptoms seen after concussion. Identifying such patients meant that they could be routed much more quickly to Advance Practice Nurses and Physicians’ Assistants to initiate such treatment quickly. Recognizing the intersection and overlap of PTSD and TBI symptoms, as well as which symptoms remain unique to each disorder also proved critical in the appropriate treatment responses to these injuries. Results were also consolidated into briefings for the combat units pending further deployments, such as the following briefings given by the senior author to the 4th Infantry Division.
Upon completion of this project, the senior author was designated both OIC of the newly formed CRDAMC Traumatic Brain Injury Clinic and was also named liaison Officer between CRDAMC and the Defense Veterans’ Brain Injury Center (DVBIC). DVBIC serves active-duty military, their beneficiaries, and veterans with traumatic brain injury through state-of-the-science clinical care, innovative clinical research initiatives and educational programs, and support for force health protection services. DVBIC was the TBI operational component of the Defense Centers of Excellence (DCoE) for Psychological Health and Traumatic Brain Injury and has since been rebranded as the TBI Center of Excellence. The third author was assigned to duties at the newly formed Triage Center for the R&R Clinic, where he oversaw the screening and triage of hundreds of injured Soldiers. Over the next six years, all authors assisted in the management of the CRDAMC Traumatic Brain Injury Clinic and the R&R as well as the ongoing collection of further research data related to TBI. These findings were eventually incorporated into treatment protocols for injured Soldiers, and contributed to the eventual writing of the VA/DoD Clinical Practice Guideline For Management Of Concussion/ Mild Traumatic Brain Injury,27 the official guidelines for the diagnosis and management of TBI for the military,36 and motor vehicle operations guidelines after TBI injury for the military.37 The Clinic founded by the authors eventually developed into the National Intrepid Center of Excellence located at Carl R. Darnall Army Medical Center, a far cry from screening re-deploying Soldiers in the waiting room of the “old Restoration and Resilience building!”
The National Intrepid Center of Excellence Satellite Center at Fort Hood opened its doors to patients for the first time Jan. 11, 2016, moving from the senior author’s modular buildings and ushering in a new era of care on Post. The 25,000-square-foot facility includes state-of-the-art technology, a fully functioning gym, a yoga and meditation area, group session rooms, and an outdoor patio. The staff of health care and mental health professionals was reinvigorated after the Hasan attacks by the senior author. The Center continues to offer the same multidisciplinary, holistic approach to treating TBI, PTSD and other conditions as when it was initially founded by the senior author, these indications of excellence not having changed.
The National Intrepid Center of Excellence Satellite Center at Fort Hood is now the fifth of its kind on military installations across the country, all part of a joint effort by the government and the private sector.
References
- Ragland, J. (6 December 2009).“Tested by tragedy, Fort Hood family of civilians and soldiers deserve Texan of the Year honor”.The Dallas Morning News. Retrieved 4 May 2013.
- Hopewell, C. A. (1982). Neuropsychology in the U.S. Army Europe. European Medical Bulletin, 39, October, (10), 9-15.
- Blast Injuries: Essential Facts. National Center for Injury Prevention and control; Division or Injury Response. U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. CS218119-A).
- Levin, H.S., Mattis, S., Ruff, R.M., Eisenberg, H.M., Marshall, L.F., Tabaddor, K., High Jr,W. M., Frankowski R.F., (1987). Neurobehavioral outcome following minor head injury: a three-center study. Journal of Neurosurgery, Feb; 66 (2): 234-43.
- Bleiberg, J., Cernich, A., & Reeves, D. (2006). Sports Concussion Applications of the Automated Neuropsychological Assessment Metrics Sports Medicine Battery. In R. J. Echemendía (Ed.), Sports neuropsychology: Assessment and management of traumatic brain injury (pp. 263–283). The Guilford Press.
- Arciniegas, D. B., Anderson, C. A., Topkoff, J., & McAllister, T. W. (2005). Mild traumatic brain injury: A neuropsychiatric approach to diagnosis, evaluation, and treatment. Neuropsychiatric Disease and Treatment, 1(4), 311–327.
- Levin, H. S., Eisenberg, H. M., and Benton, A. L, (Eds.) (1989). Mild Head Injury. Oxford University Press, New York/ Oxford.
- Klein, R., Hopewell, C.A., & Kennedy, J. (2012). Empirical Assessment of the Neurobehavioral Symptom Inventory to Determine Construct Validity of Postconcussion Syndrome. Poster presentation at the meeting of the American Academy of Clinical Neuropsychology: Seattle, WA.
- Trudeau, D., Anderson, J., Hansen, L., Shagalov, D. N., Schmoller, J., Nugent, S., and Barton, S., (1998). Findings of Mild Traumatic Brain Injury in Combat Veterans With PTSD and a History of Blast Concussion. Journal of Neuropsychiatry. Volume 10, Issue 3, August, 308-313.
- Spitzer, R., L., First, M., B., and Wakefield, J., C. (2007). Saving PTSD from itself in DSM-V. Journal of Anxiety Disorders, Volume 21, Issue 2, 233-241.
- Gold, S., D, Marx, B., P, Soler-Baillo, J., M., and Sloan, D., M. (2005). Is life stress more traumatic than traumatic stress? Journal of Anxiety Disorders. 19 (6): 687-98.
- Boals, A. and Schuettler, D. (2009). PTSD symptoms in response to traumatic and non-traumatic events: the role of respondent perception and A2 criterion. Journal of Anxiety Disorders. May;23(4):458-62.
- Kennedy, J. E., Jaffee, M.S., Leskin, G. A., Stokes, J. W., Leal, F. O., and Fitzpatrick, P., J. (2007). Posttraumatic stress disorder and posttraumatic stress disorder-like symptoms and mild traumatic brain injury. Journal of Rehabilitation Research and Development. Vol 44, N: 7, 895 – 920.
- Stein, M, B. and McAllister, T. W. (2009). Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. American Journal of Psychiatry. Jul;166 (7): 768-76.
- Stahl, S. (2008). Stahl’s Essential Psychopharmacology: Neuroscientific Basis and Practical Applications, Third Edition. Cambridge University Press: New York.
- Glaesser, J., Neuner, F., Lütgehetmann, R., and Elbert, T. (2004). Posttraumatic stress disorder in patients with traumatic brain injury. BMC Psychiatry, 4 Article No 5, March 9.
- Benge, J. F., Pastorek, N., J., and Thornton, G. M. (2009). Postconcussive symptoms in OEF-OIF veterans: factor structure and impact of posttraumatic stress. Rehabilitation Psychology. Aug; 54 (3): 270-8.
- Blanchard, E., B., Jones-Alexander, J., Buckley, T., C., and Forneris, C. A. (1996).
- Bovin, M. J., Marx, B., P. et al. (2016). Psychometric Properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in Veterans. Psychological Assessment In the public domain, Vol. 28, No. 11, 1379 –1391.
- Klein, R., Hopewell, C.A., & Kennedy, J. (2012). Empirical Assessment of the Neurobehavioral Symptom Inventory to Determine Construct Validity of Postconcussion Syndrome. Poster presentation at the meeting of the American Academy of Clinical Neuropsychology: Seattle, WA.
- Vanderploeg, R. D., Cooper, D., B., Belanger, H., G., Donnell, A. J., Kennedy, J. E., Hopewell, C., A., and Scott S. G. (2014). Screening for postdeployment conditions: development and cross-validation of an embedded validity scale in the neurobehavioral symptom inventory. The Journal of head trauma rehabilitation 29 (1), 1-10.
- Iverson, G., Gaetz, M., Lovell, M., & Collins, M. (2004). Cumulative effects of concussion in amateur athletes. Brain Injury, 18(5), 433-443.
- Levin, H., Amparo, E., Eisenberg, H., Williams, P., High, W., McArdle, C. & Weiner, R. (1987). Magnetic resonance imaging and computerized tomography in relation to the neurobehavioural sequalae of mild and moderate head injury. Journal of Neurosurgery, 66, 706-713.
- Lishman, W. (1988). Physiogenesis and psychogenesis in the post-concussional syndrome. British Journal of Psychiatry, 153, 460-469.
- Bazarian, J., Wong, T., Harris, M., Leahey, N., Mooherjee, S., and Dombovy, M. (1999). Epidemiology and predictors of post-concussion syndrome after minor head injury in an emergency population. Brain Injury, 13, 173–189.
- Iverson, G., Brooks, B., Lovell, M., & Collins, M. (2006). No cumulative effects for one or two previous concussions. British Journal of Sports Medicine, 40(1), 72-75.
- VA/DoD CLINICAL PRACTICE GUIDELINE FOR MANAGEMENT OF CONCUSSION/ MILD TRAUMATIC BRAIN INJURY. Department of Veterans Affairs/ Department of Defense. Prepared by: The Management of Concussion/mTBI Working Group With support from: The Office of Quality and Performance, VA, Washington, DC & Quality Management Directorate, United States Army MEDCOM Version 1.0 – 2009.
- Moore, B., A., Hopewell, C., A., and Grossman, D. (2009). Violence and the warrior, In Living and Surviving In Harm’s Way: A Psychological Treatment Handbook for Pre- and Post-Deployment. S. M. Freeman B. A. Moore, and A. Freeman, (Eds.) Routledge: New York.
- Radloff, L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
- Christopher, R., Reiman, J., and Hopewell C. A., (1997). Traumatic Event Sequelae Inventory. Military trauma assessment TESI-mt.
- Lewinsohn, P. M., Seeley, J. R., Roberts, R. E., & Allen, N. B. (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12(2), 277–287.
- Pinquart, M., & Sörensen, S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18(2), 250–267.
- Roth, D.L., Ackerman, M. L., Okonkwo, O. C., & Burgio, L. D. (2008). The four-factor model of depressive symptoms in dementia caregivers: A structural equation model of ethnic differences. Psychology and Aging, 23, 567–576.
- California CLAIMS Journal, Winter 1996.
- Christopher, R. and Hopewell, C. A. (2007). Psychiatric correlates of combat trauma in military personnel: PTDS and TBI TESI statistical analysis. Operation Iraqi Freedom and Operation Enduring Freedom. ISBN 158028-16-4. Reno, Nevada: Psychological, Clinical, and Forensic Assessment.
- McCrea, M., Pliskin, N., Barth, J., Cox, D., Fink, J., French, L., Hammeke, T., Hess, D., Hopewell, C. A., Orme, D., Powell, M., Ruff, R., Schrock, B., Terryberry-Spohr, L., Vanderploeg, R., Yoash-Gantz, R. (Jan 2008). Official position of the military TBI task force on the role of neuropsychology and rehabilitation psychology in the evaluation, management, and research of military Veterans with traumatic brain injury. The Clinical Neuropsychologist, 22 (1) 10 – 26.
- Driving Following Traumatic Brain Injury: Clinical Recommendations (This is the actual Clinical Practice Guideline for Driving for the Unites States Army, signed off on by BG Lorree Sutton). Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury. Driving Evaluations after Traumatic Brain Injury Conference. 28 July 2009, Washington, DC.
ABOUT THE AUTHOR

Dr. Alan Hopewell holds four degrees and four foreign language certifications, to include his BS, MS and PhD in Clinical Psychology and a second Master of Science Degree in Clinical Psychopharmacology.
He received his formal Clinical Neuropsychological training during his residency at the University of Texas Medical Branch in Galveston in the Division of Neurosurgery where he was the very first student of Harvey Levin, PhD, ABPP.
Dr. Hopewell was commissioned upon his graduation from the Texas A&M Corps of Cadets. He has served as Chief of Psychology Service at Landstuhl Army Regional Medical Center, where he founded the initial Traumatic Brain Injury Laboratory and at Brooke Army Medical Center, among others. He was the first Army Officer Prescribing Psychologist to serve and to practice in a Combat Theater, where he was awarded the Bronze Star Medal for meritorious service during Operation Iraqi Freedom. He was subsequently awarded a Meritorious Service Medal as he was a primary target during the Ft. Hood Jihadist Terrorist attack by his colleague, Nidal Hasan.
A former president of the Texas Psychological Association, he was also Awarded the Texas Psychological Association Award as the Outstanding Clinical Neuropsychologist in Texas.
He is currently Assistant Professor of Psychiatry and Behavioral Medicine, University of North Texas Health Science Center and maintains his practice in Fort Worth. He has been married for 48 years, has two sons, and is just now expecting his first grandson. His father, LTC Clifford Hopewell, a B-17 navigator prisoner of war, was the stenographer for the infamous Stalag Luft III prison camp in Germany (The Great Escape).
Based upon his combat service and as a prescribing psychologist, he was awarded one of the highest honors of the American Psychological Association, being elected a Fellow of the APA. He is currently an Assistant Professor of Psychiatry and Behavioral Medicine at the University of North Texas Health Science Center.
Dr. Robert Klein is a former Army psychologist with a PhD in clinical psychology. He is currently in private practice and conducts research involving active-duty military personnel and Veterans. His research publications and professional presentations focus on statistics and neuropsychology. Prior to becoming a psychologist, he was an US Army Airborne Ranger and qualified Infantryman. During his infantry time, he served on the Korean DMZ. Dr. Klein is also an OIF II Veteran.
military personnel and Veterans. His research publications and professional presentations focus on statistics and neuropsychology. Prior to becoming a psychologist, he was an US Army Airborne Ranger and qualified Infantryman. During his infantry time, he served on the Korean DMZ. Dr. Klein is also an OIF II Veteran.
Michael L. Adams, PhD, LTC (RET) – I was born into a military family. My paternal grandfather was a Soldier in the Army of the Czar of Russia. He and my grandmother escaped from the old country by hiding in a hay wagon. He bribed the guards to miss them when the guards stabbed the hay with bayonets. They emigrated to America around the turn of the last century. My father was born in the United States of America. When he was fifteen, he came home from school to learn his last name had been legally changed from Abramov to Adams. As a child, he remembered folding bandages for wounded Soldiers from WW I. When he was in college, he joined ROTC. He attended law school and undergraduate college simultaneously, graduating with a law degree before he graduated with his undergraduate degree. When WW II began, he commanded a coast artillery battery and later went to Europe as an intelligence officer. While in Europe, he was blown up in the air by a V-1 bomb. He flew on missions with B-17 bomber crews and had shrapnel pierce his helmet and travel around inside it, while missing his skull. He never talked much about his experiences, especially during the Korean War.
emigrated to America around the turn of the last century. My father was born in the United States of America. When he was fifteen, he came home from school to learn his last name had been legally changed from Abramov to Adams. As a child, he remembered folding bandages for wounded Soldiers from WW I. When he was in college, he joined ROTC. He attended law school and undergraduate college simultaneously, graduating with a law degree before he graduated with his undergraduate degree. When WW II began, he commanded a coast artillery battery and later went to Europe as an intelligence officer. While in Europe, he was blown up in the air by a V-1 bomb. He flew on missions with B-17 bomber crews and had shrapnel pierce his helmet and travel around inside it, while missing his skull. He never talked much about his experiences, especially during the Korean War.
On my mother’s side of the family, I know one uncle served in WW II. He fought in the Pacific and was affected by night hand to hand combat with Japanese soldiers. He told me how to fight with a knife as he had done.
I was the middle child of three. With a family background of military service, I was expected to join the military. In college I joined Air Force ROTC just as my brother had before me. I graduated with designation Distinguished Military Graduate in 1966. I entered active duty in January 1968 and was ordered to Intelligence Officer School, where I was invited to accompany the commander to Southeast Asia. I was stationed in Thailand where I was part of electronic interdiction of traffic on the Ho Chi Minh Trail, which extended from North Vietnam through Laos to South Vietnam. This was the main route of people and supplies for the communists. We were operating in real time ambushing enemy convoys and people as they travelled south. I also joined a flying unit, the Airborne Battlefield Command and Control Squadron and flew about 800 hours of combat. I provided support for our allies on the ground in Laos.
After my time in the war, I was assigned to Strategic Air Command (SAC). I became Officer in Command (OIC) of a cartographic section making air target charts. There were about 25 people in my section. I re-organized us so each of the senior sergeants was able to step up and run the section. There were no vital individuals whose absence would cause work to stop. There were just two ways to leave SAC – either leave the Air Force or die. I left and went to graduate school to study psychology. I was told the Army would pay me to go to school, so I applied and was one of fifteen people that year to become Army graduate students.
My first assignment was to the Academy of Health Sciences as an instructor. I created some instructional materials about human development before there were any textbooks that I could find. I also helped create a course to lower stress in nursing anesthetist officers. I taught assertiveness to Army nurses. I went to William Beaumont Army Medical Center for internship after two years at the Academy.
The internship is where we began to identify what became called post-traumatic stress disorder (PTSD) in Soldiers who had been in combat in Vietnam. We began to develop treatments to restore the Soldiers to full functioning. This was a lot harder back then because we did not grasp the complexity of the condition. Sometimes experts were brought to the Internship to educate us. I remember well that the chief of psychiatry from the Israeli Army spoke to us about the Six Day War and how quickly PTSD developed as well as what they did to reduce PTSD. We were astonished and asked how they developed the treatment. He looked puzzled and then told us the Israeli mental health people copied our procedures from the Korean War. None of us knew of the Korean War procedures. By the time of the Vietnam War, we had forgotten our own history.
My next assignment was to Combat Developments at Fort Benjamin Harrison. The most important contribution there was when I became curious about continuous operations. I reviewed twenty years of research in continuous operations and reduced it to two paragraphs for a General Officer talking paper. After it was presented at a conference, changes were made so that our Soldiers would have enough water to drink. Another doctrine change was about how often to drink water. These changes allowed our Soldiers to fight in the Gulf War in 1991 for longer than 45 minutes, which is how long the fight could go on under the previous doctrine of water conservation.
From Combat Development, I was assigned as the Division Psychologist for the 25th Infantry Division. There we noticed that whenever deploying Soldiers were boarding aircraft to go to South Korea for an exercise, some Soldiers would get to the bottom of the aircraft ramp, suddenly drop their packs and rifles, and RUN AWAY. Looking further, we found ALL of them were Vietnam Combat Veterans. We were able to get their commanders to send them to Mental Health for help instead of punishing these Soldiers. We stayed busy. I also wrote a proposal for computer communication between the medical center and our mental health at Schofield Barracks in Hawaii so we could ensure continuity of care. Prior to that, Soldiers would be discharged from psychiatry and returned to their units, with no follow up at all.
From Schofield Barracks I moved to Fort Hood’s Carl R Darnall Army Community Hospital to the Department of Psychiatry. I left active duty and became a school psychologist for the Copperas Cove School District in Texas. There I developed an autism assessment team and also maintained the functioning of three self-contained classrooms for children with severe behavioral problems. I stayed there for seven and a half years and until being called back to active duty for Operation Desert Storm. I stayed with the Army hospital for most of the next 19 years, treating many more Soldiers who had deployed to the wartime theater and their family members. At the age of 60, I retired from the Army, but returned as a volunteer for three more years in 2005, serving as chief of the Department of Psychology and chief of the combined departments of behavioral health. This included departments of psychiatry, psychology, social work, and substance abuse treatment. This was an exciting time for high-speed change. My life became more intense after former Major Hasan massacred 14 people at Fort Hood on 5 November 2009. I estimate I treated over 4,000 Soldiers for PTSD from 1978 until I finally retired in 2015.
Combat Stress Magazine
Combat Stress magazine is written with our military Service Members, Veterans, first responders, and their families in mind. We want all of our members and guests to find contentment in their lives by learning about stress management and finding what works best for each of them. Stress is unavoidable and comes in many shapes and sizes. It can even be considered a part of who we are. Being in a state of peaceful happiness may seem like a lofty goal but harnessing your stress in a positive way makes it obtainable. Serving in the military or being a police officer, firefighter or paramedic brings unique challenges and some extraordinarily bad days. The American Institute of Stress is dedicated to helping you, our Heroes and their families, cope with and heal your mind and body from the stress associated with your careers and sacrifices.